Obesity or Overweight Now Affect 1 in 3 Youth: How Experts Are Responding

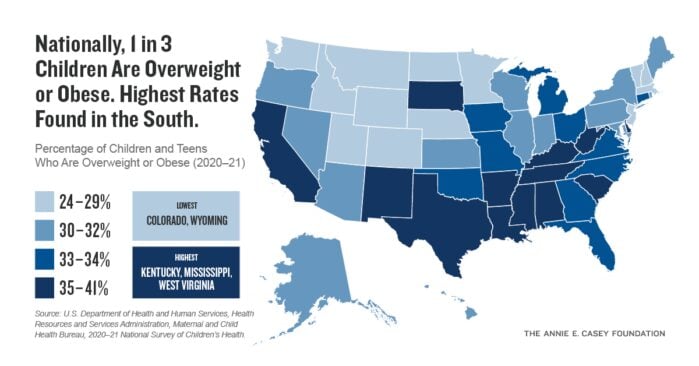
One in three youth ages 10 to 17 experience obesity or overweight, according to newly updated data in the Annie E. Casey Foundation’s KIDS COUNT® Data Center. The latest 33% figure in 2020–2021 represents an increase of 2 percentage points in five years and corresponds with an increasing share of youth who do not exercise regularly (55% in 2020–2021).
Obesity alone affects 14.4 million children and teens nationwide and has become a leading chronic disease among kids, according to the American Academy of Pediatrics (AAP). Obesity also increases the risk of other serious physical and mental health conditions, including:
- Heart disease
- Type 2 diabetes
- Asthma
- Anxiety
- Depression
The Medical Field’s Evolving Views on Obesity
Defined as having a Body Mass Index at or above the 95th percentile for age, obesity is no longer considered a result of individual choices but, instead, a complex disease resulting from socioeconomic, environmental and genetic factors, as described in new clinical guidelines from the AAP. In particular, adversity during childhood, such as poverty and racism, can affect health in critical ways and increase the risk for obesity. The AAP now recognizes the central role that social determinants of health play in childhood weight — that is, children’s experiences, social contexts and access to resources greatly influence their likelihood of having an unhealthy weight.
Disparities in Youth Obesity and Overweight
Given the influence of structural inequities and sociocultural factors on health, overweight and obesity do not affect all children equally. For instance:
- The 2023 KIDS COUNT Data Book reports that rates of obesity or overweight were substantially higher for Latino (43%) and Black (40%) youth compared to white (27%) and Asian and Pacific Islander youth (24%) in 2020–2021. Over the past three years, rates jumped by 6 percentage points for Asian and Pacific Islander youth and 5 percentage points for Latino youth, the largest increases of all racial and ethnic groups with data.
- The AAP states that overweight and obesity are more prevalent among kids living in poverty, low-resource communities and immigrant families, as well as those who have experienced discrimination or stigma.
- Looking across the country in 2020–2021, the highest rates of youth obesity or overweight were generally found in southern states, with 41% in Kentucky, Mississippi and West Virginia, while Colorado and Wyoming had the lowest rates in the nation, at 24%. Notably, rates increased in 35 states over the last five years, with some rates rising by an alarming 9 or 10 percentage points.
- When examining national rates by gender, males ages 10 to 17 consistently had higher rates of obesity or overweight than their female peers over the last five years — reaching 36% versus 31%, respectively, in 2020–2021. Potential reasons for this difference: Male youth typically spend more time on digital devices and may be more vulnerable to food and beverage marketing than females, according to the AAP.
Body Mass Index (BMI) Is a Limited Measure
While most indicators of childhood obesity or overweight come from BMI, it is important to recognize that this simply measures body size and weight, rather than actual health based on metabolic or other measures. Being a larger size does not necessarily mean one is unhealthy, and labeling children as overweight or obese based on their BMI can cause psychological harm.
Further, as described in a recent report by the Robert Wood Johnson Foundation, BMI is based on Euro-American body types and does not take into account race or ethnicity. The report states, “There is no universal ideal body nor a single size for good health. We need to move beyond a weight-centered view of health, and avoid shaming and blaming those living in large bodies.” Going forward, it will be critical to improve methods of assessing children’s weight and health.
Changing Approaches to Childhood Obesity Prevention and Treatment
Increasingly, many leaders and sectors are using systemic solutions to tackle the deep-rooted, structural forces behind the rise in childhood obesity and the disparities by race and socioeconomic status. Examples include improving access to nutritious and affordable food, especially in low-income communities, and ensuring that all families have adequate resources to support their children’s health. Other solutions involve making improvements in schools and built environments, including increased opportunities for exercise, as well as addressing food and beverage marketing to young people.
The AAP has responded to this concerning trend with new clinical practice guidelines for pediatric obesity treatment, based on the latest evidence. Fundamentally, the guidelines state that treatment should be comprehensive, long-term and in the context of a medical home, using a chronic care model with family-centered and non-stigmatizing approaches. More specific recommendations differ by age group:
- For ages 2 and older: Treatment can include intensive behavioral, nutrition and physical activity support, with active parental and family engagement.
- For ages 12 and older: Treatment can include weight loss pharmacotherapy, in addition to behavioral and lifestyle support.
- For ages 13 and older with severe obesity: Physicians can refer teens for evaluation for metabolic and bariatric surgery, in addition to the above options.
Unfortunately, many children cannot access or afford evidence-based treatment or high-quality health care generally. Given this, the AAP also recommends promoting “supportive payment and public health policies that cover comprehensive multicomponent obesity prevention, evaluation, and treatment, including policy changes within and beyond the health care sector.” Ensuring that all families have access to affordable, comprehensive health insurance and care has long been a priority among those working to improve children’s health. Additional AAP recommendations include combatting structural racism and expanding access to effective community programs and resources.
As childhood obesity rates continue to increase, and disparities endure, much more work is needed to advance prevention, treatment and data collection efforts.
More About Child Health and Equity Issues
- Read the 2023 KIDS COUNT Data Book, which tracks the overweight or obesity indicator.
- See all data on the KIDS COUNT Data Center, including health, demographic, economic and family indicators.
- Explore the Casey Foundation’s equity and inclusion resources.
- Visit the Robert Wood Johnson Foundation’s State of Childhood Obesity website.
Sign up for our newsletters to get the latest reports and resources





